Introduction to the Retatrutide Mechanism of Action
Retatrutide is an investigational peptide that has attracted attention because it acts through multiple hormonal pathways rather than a single receptor. Most people who are familiar with therapies such as Semaglutide or Tirzepatide will know that these are incretin-based drugs, meaning they mimic natural gut hormones released after eating. Retatrutide takes this further by working as a tri-agonist and engaging three different receptor systems that together influence how the body regulates energy, glucose, and appetite.
At its foundation, Retatrutide fits within the incretin therapy category. Incretins like GLP-1 are normally secreted in response to food intake, helping stimulate insulin, regulate blood sugar, and send signals of satiety to the brain. Synthetic molecules designed to mimic these hormones have been effective in both diabetes and obesity care, but they are usually limited to one or two receptors. Retatrutide was designed to push beyond this by activating GLP-1 receptors, GIP receptors, and glucagon receptors all at once. This combination means the drug has the potential to blend benefits from three overlapping but distinct biological systems.
The GLP-1 pathway is the most widely studied and is central to many current treatments. It slows down how quickly food leaves the stomach, enhances insulin release when glucose is present, and communicates with areas of the brain that reduce appetite. The GIP pathway works in a similar way to promote insulin secretion, and while its independent effects have sometimes been debated, when combined with GLP-1 activation it appears to create an additive response. The glucagon receptor is a different case. On its own, stimulating glucagon would raise blood sugar, but when balanced carefully alongside GLP-1 and GIP activity, it contributes to increased energy expenditure and fat breakdown. Researchers believe this is part of why Retatrutide has shown strong weight-reducing effects in early studies.
Because of this multi-receptor activity, Retatrutide is sometimes referred to as a next-generation incretin therapy. Rather than acting only on food intake or only on insulin control, its mechanism aims to work on both sides of the metabolic equation: reducing energy coming in through appetite control, and increasing energy use through glucagon-driven expenditure. This dual action is paired with improvements in blood sugar handling through insulin pathways. The result is a candidate drug that could address several interconnected problems at the same time, including obesity, type 2 diabetes, and metabolic dysfunction.
At the same time, this complexity also means that scientists are paying close attention to how Retatrutide behaves in human trials. Combining three receptor systems requires a careful balance to avoid overstimulation, and the long-term consequences are not yet fully understood. Nevertheless, the rationale is clear: by uniting these pathways into one therapy, Retatrutide may achieve greater metabolic improvements than single-pathway drugs have managed. This introduction sets the stage for looking more closely at each receptor target, the downstream metabolic pathways, and the broader implications of the Retatrutide mechanism of action.
Ready to Order?
Choose your preferred amount below, fast shipping and secure checkout.
-
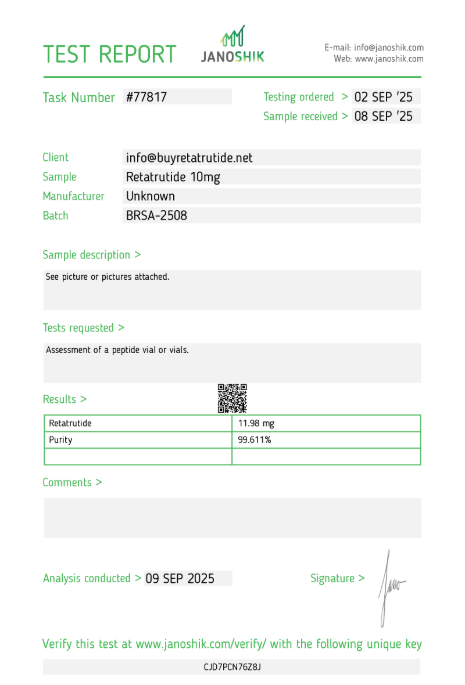
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
How Retatrutide Targets Receptors
The Retatrutide mechanism of action is unique because it engages three different receptor systems at once: GLP-1, GIP, and glucagon receptors. Each receptor has its own role in regulating metabolism, and the way Retatrutide interacts with them is central to its potential benefits. Instead of acting in isolation, the molecule is designed to mimic natural hormones and bind selectively to each target in a way that promotes complementary outcomes.
The GLP-1 receptor is perhaps the most familiar. It is expressed in the pancreas, gastrointestinal tract, and brain. When activated, it slows gastric emptying, increases insulin release in response to glucose, and reduces food cravings through appetite control centres. Retatrutide acts here much like existing GLP-1 drugs, but it does so in combination with other pathways that enhance the effect. This ensures more stable blood glucose levels and helps suppress overeating, which has been shown to drive meaningful weight reduction in early studies.
The GIP receptor is the second target. GIP is another incretin hormone that is released by the small intestine after eating. It has historically been considered less effective than GLP-1 alone, but recent research shows that when GIP and GLP-1 are activated together, they may create an additive or even synergistic effect. Retatrutide binds to the GIP receptor to enhance insulin secretion and improve the body’s sensitivity to glucose. This may help overcome one of the limitations of single-pathway drugs, giving it an edge in treating both obesity and diabetes.
The third receptor, glucagon, presents a different challenge. Normally, stimulating the glucagon receptor would increase glucose release from the liver, which seems counterproductive for diabetes care. However, when carefully balanced alongside GLP-1 and GIP activation, glucagon signalling can increase energy expenditure and fat breakdown. Retatrutide has been engineered to harness this effect while still keeping blood sugar under control. The balance is delicate, but when achieved, it can result in greater overall energy burn without destabilising glucose regulation.
By combining these three receptor actions into one therapy, Retatrutide attempts to replicate a more natural and holistic hormonal response to food intake. Instead of only focusing on reducing appetite or only on lowering glucose, it simultaneously addresses multiple arms of metabolism. This multi-targeting strategy may explain why clinical studies so far have shown larger reductions in both body weight and glucose markers than would be expected from GLP-1 therapy alone. The design represents a step forward in incretin-based drug development, aiming to treat metabolic disease in a more comprehensive way.
Metabolic Pathways Affected
Retatrutide influences several key metabolic pathways through its simultaneous action on GLP-1, GIP, and glucagon receptors. These receptors are deeply integrated into the body’s control systems for blood sugar, appetite, and energy use. By activating all three together, Retatrutide is able to modify not just one, but multiple aspects of metabolism, which explains its wide-ranging effects in clinical studies.
One of the most direct pathways affected is glucose regulation. The GLP-1 and GIP receptors both act in the pancreas to enhance insulin secretion in response to meals. This makes it easier for the body to move glucose out of the bloodstream and into cells, where it can be used for energy. At the same time, GLP-1 reduces the release of glucagon from the pancreas, helping prevent unnecessary glucose release from the liver. Retatrutide’s dual incretin activity strengthens this regulation, creating tighter post-meal glucose control.
Another important pathway is energy intake, which is largely controlled by the brain and gut. GLP-1 receptor activation slows gastric emptying and transmits satiety signals to appetite centres, reducing the desire to continue eating. GIP receptor activation may also contribute to satiety, though its role is less well defined. Together, these actions reduce calorie consumption without the need for conscious restriction, a factor that has been critical in the observed weight reductions seen in trials.
The glucagon receptor contributes to energy expenditure, which is where Retatrutide differs most from older GLP-1-only therapies. By stimulating this receptor, the liver increases the breakdown of stored fat and slightly elevates glucose output. On its own, this would be problematic, but when paired with GLP-1 and GIP activation, it leads to an overall increase in energy burn without destabilising blood sugar. This balance is thought to improve fat metabolism while supporting weight reduction goals.
Beyond glucose and weight regulation, Retatrutide’s influence may extend into lipid metabolism and cardiovascular health. Early trial data suggest improvements in cholesterol levels and markers of heart health, which may stem from its impact on fat breakdown and energy balance. While further studies are needed, the ability to alter multiple metabolic pathways at once points to a therapy that could offer comprehensive benefits in conditions where obesity, diabetes, and cardiovascular risk are closely linked.
Altogether, the metabolic effects of Retatrutide highlight why researchers are considering it a next-generation incretin therapy. By reducing food intake, improving glucose control, and increasing energy expenditure, it addresses both sides of the energy balance equation. This contrasts with many existing therapies that focus narrowly on either intake or expenditure. It is this broad pathway involvement that sets Retatrutide apart as a potential tool for treating complex metabolic diseases.
Impact on Glucose Regulation
One of the most important aspects of the Retatrutide mechanism of action is its influence on glucose regulation. In people with obesity or type 2 diabetes, blood sugar levels often remain elevated because the body does not produce or respond to insulin effectively. Retatrutide addresses this problem by activating GLP-1 and GIP receptors in the pancreas, which directly increase insulin secretion in a glucose-dependent manner. This means insulin is released only when blood sugar levels are high, lowering the risk of hypoglycaemia while improving post-meal glucose handling.
GLP-1 activation also reduces glucagon release from pancreatic alpha cells. Glucagon is a hormone that normally triggers the liver to release glucose into the bloodstream. By keeping this in check, Retatrutide prevents unnecessary rises in blood sugar after meals. At the same time, its GIP activity further enhances insulin sensitivity in muscle and fat tissues, ensuring that circulating glucose can be absorbed and used more effectively for energy rather than remaining in the bloodstream.
The addition of glucagon receptor activity might seem contradictory, because glucagon stimulation typically raises blood sugar. However, when paired with GLP-1 and GIP activation, the balance shifts toward improved energy expenditure without uncontrolled spikes in glucose. Early studies show that the net effect of Retatrutide is better overall glycaemic control compared to traditional single-pathway therapies. Patients in clinical trials demonstrated significant reductions in fasting glucose, as well as improved HbA1c, which is a key measure of long-term blood sugar regulation.
Another key factor is gastric emptying. By slowing the rate at which food leaves the stomach, GLP-1 receptor activation helps prevent sharp spikes in blood sugar following meals. This steady release of nutrients allows the pancreas and liver to manage glucose more smoothly. For people with insulin resistance, this is particularly valuable because it reduces the burden on beta cells and prevents the cycle of post-meal surges that can worsen diabetes over time.
Together, these actions create a multi-layered defence against dysregulated blood sugar. Increased insulin secretion, reduced glucagon, slower gastric emptying, and improved tissue uptake all contribute to stabilised glucose levels. This comprehensive approach is one of the main reasons Retatrutide is considered a strong candidate for treating both type 2 diabetes and obesity, where glucose handling is central to overall health outcomes.
Effects on Appetite and Weight
Retatrutide’s impact on appetite and body weight is one of the most closely studied outcomes in its clinical trials. Obesity is driven by a combination of excess calorie intake and impaired metabolic efficiency, and Retatrutide addresses both sides of this equation. Its GLP-1 receptor activity plays a central role by slowing gastric emptying and sending satiety signals from the gut to the brain. This reduces the desire to continue eating after meals and lowers the frequency of cravings between meals, creating a natural reduction in calorie intake without the need for forced restriction.
GIP receptor activation adds an additional layer of appetite control. While its effects have been debated, evidence suggests that when combined with GLP-1 signalling, GIP may improve the sensation of fullness and reinforce the body’s ability to self-regulate food intake. Together, these incretin pathways reduce the likelihood of overeating, which is a crucial factor in long-term weight management. Patients in early trials often reported feeling satisfied with smaller meals, highlighting the practical effects of these mechanisms.
In parallel, Retatrutide’s glucagon receptor activity enhances energy expenditure. By modestly stimulating glucagon pathways, the drug encourages the body to break down fat stores and increase metabolic rate. This helps shift the balance from energy storage toward energy use. The combined reduction in calorie intake and increase in calorie burn is thought to underpin the strong weight loss results observed in trials, where patients achieved double-digit percentage reductions in body weight over extended periods.
Another important element is the effect on eating behaviour. By reducing hunger signals and enhancing satiety, Retatrutide lowers the psychological burden often associated with dieting. Patients are less likely to feel deprived, which improves adherence and supports more sustainable weight loss. This makes it different from many traditional weight-loss strategies that rely heavily on willpower and calorie counting, both of which often fail in the long run.
Collectively, these appetite- and weight-related effects show that Retatrutide is not only a glucose-lowering therapy but also a potential tool for addressing obesity at its root. By combining control over food intake with increased fat metabolism, it offers a comprehensive approach to weight management that goes beyond what is typically achievable with lifestyle changes or single-pathway drugs alone.
Comparison with Other GLP-Based Therapies
Retatrutide is often compared to established GLP-1 receptor agonists such as semaglutide and liraglutide, as well as the dual agonist Tirzepatide. While all of these therapies are part of the incretin family, Retatrutide stands out because it targets three receptor systems simultaneously. This tri-agonist profile differentiates it not only in terms of mechanism but also in terms of potential outcomes for patients managing diabetes, obesity, or both.
GLP-1 agonists like semaglutide primarily influence appetite and glucose regulation by slowing gastric emptying, enhancing insulin secretion, and reducing glucagon release. These drugs have demonstrated strong weight reduction and improved glycaemic control, but their activity is confined to a single pathway. In contrast, Retatrutide adds two more layers of activity through GIP and glucagon receptor engagement. This expands its potential to influence both energy intake and energy expenditure in ways that single-pathway drugs cannot achieve.
Tirzepatide, a dual agonist targeting GLP-1 and GIP, provides a useful benchmark. It has shown stronger weight loss and glycaemic improvements than GLP-1 drugs alone, confirming that dual incretin signalling provides a therapeutic advantage. Retatrutide extends this principle further by incorporating glucagon receptor activation. While glucagon signalling must be carefully balanced, the inclusion of this pathway introduces the potential for increased energy burn and fat metabolism, which could translate into even greater weight loss outcomes.
From a safety and tolerability perspective, Retatrutide shares some of the same considerations as other GLP-1-based therapies, particularly gastrointestinal effects such as nausea or diarrhoea. However, early trial results suggest that the addition of GIP and glucagon pathways does not necessarily increase side effect severity, though long-term data are still needed. This positions it as a therapy that could provide enhanced efficacy without substantially raising the risk profile beyond what is already observed with current incretin-based drugs.
When viewed alongside its peers, Retatrutide can be seen as the next step in incretin therapy evolution. GLP-1 agonists laid the foundation, dual agonists demonstrated the added value of targeting more than one receptor, and Retatrutide pushes further by combining three signals into a single therapy. Whether this translates into consistent superiority across diverse patient populations will depend on ongoing clinical trials, but the comparisons to date suggest it has the potential to set a new standard for metabolic treatment.
Current Research on Mechanism
Research into Retatrutide’s mechanism of action is ongoing, with most of the available evidence coming from phase 1 and phase 2 clinical trials. These studies have been designed not only to assess safety and efficacy but also to provide insights into how Retatrutide exerts its multi-receptor effects in humans. Because it acts on GLP-1, GIP, and glucagon receptors, researchers have been especially interested in understanding how these pathways interact in practice and what the net outcome looks like over time.
Clinical data so far confirm that Retatrutide improves glycaemic control and produces substantial weight loss. Patients in mid-stage trials have shown marked reductions in body weight, in some cases exceeding the results seen with existing GLP-1 or dual-agonist therapies. Detailed metabolic analyses indicate that these results are tied to a combination of increased satiety, reduced calorie intake, and enhanced fat metabolism. This aligns closely with the mechanistic hypothesis behind the drug, which aims to combine appetite regulation with higher energy expenditure.
Beyond glucose and weight outcomes, current research has also begun to examine Retatrutide’s impact on cardiovascular and metabolic risk factors. Early findings suggest improvements in lipid profiles, reductions in inflammatory markers, and favourable effects on blood pressure. While these changes are secondary to the primary endpoints, they provide valuable clues about how the drug’s broad receptor activity influences the body at a systemic level. These findings have sparked interest in whether Retatrutide could be applied beyond diabetes and obesity into related conditions such as fatty liver disease or metabolic syndrome.
Animal studies have also helped clarify some of the finer details of its mechanism. Preclinical research shows that Retatrutide’s glucagon receptor activity increases energy expenditure through hepatic and adipose tissue pathways. Meanwhile, its incretin activity reinforces insulin secretion and glucose disposal. Translating these observations to humans has required careful dose-ranging studies to ensure that the balance between glucose control and energy burn is maintained. The fact that patients in trials are demonstrating both improved glycaemic outcomes and significant weight reduction suggests that the mechanism is functioning as intended.
Despite these promising results, researchers caution that the long-term effects of sustained tri-agonist therapy are still unknown. Questions remain about durability of weight loss, potential changes in cardiovascular risk over years of treatment, and whether chronic activation of multiple receptors could introduce unforeseen side effects. Large phase 3 trials currently underway will be critical in addressing these questions and confirming whether Retatrutide’s mechanism delivers benefits that are consistent, safe, and clinically meaningful over the long term.
Safety Considerations Linked to Mechanism
Because Retatrutide engages three receptor systems simultaneously, safety considerations are closely tied to the Retatrutide mechanism of action. Each receptor pathway offers therapeutic benefits, but also brings potential risks if overstimulated. Understanding these safety aspects is essential to interpreting the drug’s potential role in future treatment strategies for diabetes and obesity.
The GLP-1 pathway, while generally well tolerated, is known to cause gastrointestinal side effects such as nausea, vomiting, and diarrhoea. These symptoms are common in many incretin-based therapies and are usually most pronounced at the start of treatment. Retatrutide shares this risk, though early clinical data suggest that gradual dose escalation can help reduce severity over time. Careful titration strategies are being studied to manage tolerability without losing efficacy.
The addition of GIP receptor activation does not appear to significantly worsen gastrointestinal effects, but it introduces its own uncertainties. Since the independent role of GIP in human metabolism is less well defined than GLP-1, researchers are monitoring long-term outcomes to ensure that sustained activation does not lead to unanticipated issues. So far, trial data suggest that GIP activity is neutral or beneficial, enhancing insulin sensitivity and contributing to weight control when paired with GLP-1 stimulation.
The glucagon receptor presents the most complex safety consideration. Normally, glucagon signalling raises blood sugar, which would be counterproductive in treating diabetes. Retatrutide is designed to balance this effect with concurrent incretin activation, but the margin for error is narrower than with GLP-1 therapies alone. If the balance were disrupted, it could theoretically result in unwanted hyperglycaemia. Clinical trials have not reported this as a major problem so far, but continued monitoring will be essential as larger populations are studied.
Another area of focus is cardiovascular safety. While early findings suggest improvements in markers such as blood pressure and cholesterol, long-term cardiovascular outcome trials are required to confirm that these translate into real-world risk reduction. Similarly, researchers are watching for signs of pancreatitis, gallbladder issues, or other complications that have been flagged as concerns with earlier incretin-based drugs. So far, no unexpected patterns have emerged, but these remain areas of caution.
In summary, the safety profile of Retatrutide appears broadly consistent with other incretin therapies, though its tri-agonist mechanism adds new dimensions that require careful study. Balancing efficacy with tolerability will be central to its development, and ongoing research is aimed at ensuring that the benefits of multi-pathway activation outweigh any risks. If trials continue to show that safety remains manageable, Retatrutide may represent a significant advance without introducing unacceptable complications.
Order Retatrutide Online
Available in 10mg vials. Select your pack size and checkout securely below.
-
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
Frequently Asked Questions
- What receptors does Retatrutide act on? Retatrutide acts on three receptors at the same time: GLP-1, GIP, and glucagon receptors. Together, these targets help regulate blood sugar, appetite, and energy use.
- How does Retatrutide influence appetite? By activating GLP-1 and GIP receptors, Retatrutide slows gastric emptying and sends signals of fullness to the brain. This reduces food cravings and helps limit calorie intake.
- Is Retatrutide’s mechanism similar to semaglutide? Retatrutide is related but not identical. Semaglutide targets only the GLP-1 receptor, while Retatrutide also activates GIP and glucagon receptors. This broader activity may provide stronger effects on weight and glucose control.
- Why does Retatrutide include glucagon receptor activity? Although glucagon usually raises blood sugar, in Retatrutide it is carefully balanced with GLP-1 and GIP activity. The result is increased energy expenditure without destabilising glucose levels.
- Are the side effects of Retatrutide different from other GLP-1 drugs? So far, trial data suggest that side effects are broadly similar, with gastrointestinal symptoms being the most common. Ongoing studies will confirm whether its tri-agonist design changes the long-term safety profile.
- How does Retatrutide help with weight reduction? It combines appetite suppression from GLP-1 and GIP signalling with increased energy expenditure driven by glucagon activity. This dual action supports significant body weight loss.
- Does Retatrutide improve insulin sensitivity? Yes. Through GIP and GLP-1 receptor activation, Retatrutide enhances insulin secretion and improves how well tissues respond to glucose, leading to better insulin sensitivity overall.
- Can Retatrutide prevent glucose spikes after meals? Yes. By slowing gastric emptying and boosting insulin release, it reduces the likelihood of sharp rises in blood sugar following meals.
- Is the effect of Retatrutide long lasting? Early data show that reductions in weight and blood sugar are sustained during treatment, but long-term durability will be confirmed in larger phase 3 studies.
- How does Retatrutide compare to Tirzepatide? Tirzepatide targets GLP-1 and GIP, while Retatrutide adds glucagon receptor activation. This difference may result in greater weight and metabolic improvements, though final outcomes will depend on trial results.
- Does Retatrutide affect cardiovascular health? Preliminary studies suggest possible improvements in cholesterol, blood pressure, and inflammation markers, but formal outcome trials are needed to confirm cardiovascular benefits.
- Is Retatrutide considered safe for long-term use? Current trials indicate a manageable safety profile similar to other incretin therapies. Long-term studies are ongoing to confirm whether extended treatment is safe.
Compare Mechanisms of Action
Triple & Dual Receptor Agonists
- Tirzepatide dual GLP-1 and GIP mechanism – Most similar to Retatrutide
- Mazdutide GLP-1 and glucagon dual agonist – Alternative dual approach
- Cotadutide dual receptor activation profile – GLP-1/GCG combination
- Survodutide mechanism of action research – Dual agonist in development
Single GLP-1 Receptor Agonists
- Semaglutide single GLP-1 receptor mechanism – Most prescribed GLP-1
- Liraglutide daily GLP-1 activation – First-generation daily injection
- Dulaglutide weekly GLP-1 receptor binding – Long-acting formulation
- Exenatide twice-daily GLP-1 mechanism – Short-acting option
Different Metabolic Mechanisms
- SGLT-2 inhibitors glucose excretion mechanism – Kidney-based approach
- Orlistat lipase inhibition for weight loss – Fat absorption blocker
- Phentermine appetite suppression mechanism – Stimulant approach
- Contrave dual neurological pathway mechanism – Brain chemistry modifier
Experimental Mechanisms in Development
- Orforglipron oral GLP-1 receptor activation – No injection needed
- Cagrisema combination semaglutide plus amylin – Dual hormone approach
- VK2735 GIP antagonist mechanism – Opposite approach to agonists
- View all experimental compound mechanisms
Research Resources
- Clinical trial results and mechanism validation
- Side effects related to mechanism
- Dosing protocols based on mechanism
- Calculate doses for research
Explore all 48 compound mechanism comparisons | Learn about proper peptide storage