Introduction
Months 2-6 represent a crucial phase in your Retatrutide treatment journey, where initial adaptation gives way to sustained therapeutic effects and long-term habit formation. This comprehensive guide covers what to expect during this extended period, including dosage adjustments, lifestyle integration, and strategies for maintaining motivation and progress.
Understanding this phase helps you navigate the transition from initial adaptation to sustained treatment success. This guide provides practical strategies, realistic expectations, and actionable advice to help you maximise your treatment outcomes during this important period. For comprehensive information about Retatrutide treatment, visit our Retatrutide Guides Hub which provides detailed guidance across all aspects of your treatment journey. If you’re just starting treatment, see our First Month Guide for initial adaptation strategies.
Ready to Order?
Choose your preferred amount below, fast shipping and secure checkout.
-
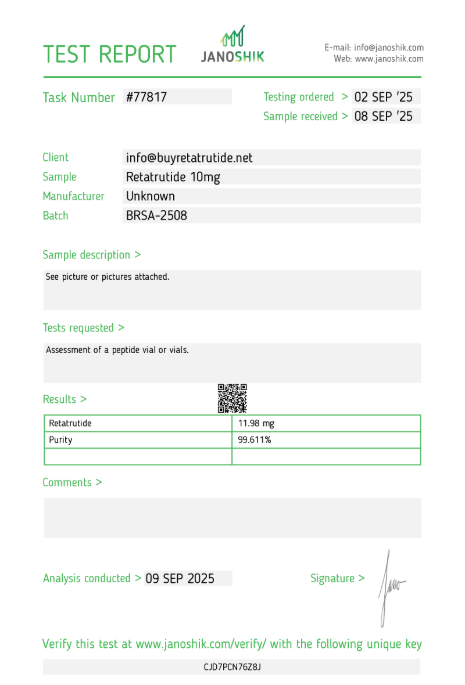
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
Month 2: Building Momentum
Month two typically marks the beginning of sustained therapeutic effects as your body becomes fully adapted to Retatrutide’s triple hormone receptor activation. Most patients experience more consistent appetite suppression, improved metabolic function, and the beginning of significant weight loss during this period.
During month two, side effects usually continue to diminish, and the medication’s beneficial effects become more pronounced and consistent. Many patients report feeling more comfortable with their treatment routine and experiencing greater confidence in their ability to manage their health goals effectively.
Appetite suppression becomes more reliable during month two, with patients reporting consistent reduction in food cravings and improved ability to control portion sizes. This effect typically becomes more stable and predictable, making meal planning and dietary adherence easier to maintain.
Energy levels often stabilise during month two, with many patients reporting improved energy and better overall mood. This is often attributed to improved blood sugar control, reduced inflammation, and the positive psychological effects of seeing progress toward their health goals.
Weight loss typically becomes more apparent during month two, with many patients experiencing steady, consistent weight loss. Individual responses vary, but most patients begin to see measurable progress that reinforces their commitment to treatment and lifestyle modifications.
Month 3: Sustained Progress
Month three often represents a period of sustained progress and stabilisation as Retatrutide’s effects become fully established. Most patients experience consistent appetite suppression, stable energy levels, and continued weight loss during this period.
During month three, patients typically develop more sophisticated strategies for managing their treatment and lifestyle modifications. This includes refined meal planning techniques, optimised exercise routines, and improved stress management strategies that support long-term success. For comprehensive lifestyle guidance, see our Diet Recommendations Guide and Exercise Guidelines.
Metabolic improvements become more apparent during month three, with many patients reporting improved blood sugar control, better cholesterol levels, and enhanced overall metabolic function. These improvements often accompany continued weight loss and contribute to overall health improvement.
Social and lifestyle integration becomes easier during month three as patients become more comfortable with their treatment routine and develop strategies for managing social situations, work commitments, and family responsibilities while maintaining their health goals.
Monitoring and tracking become more refined during month three as patients learn which metrics are most meaningful for their individual progress and develop more sophisticated approaches to tracking their health improvements and treatment effectiveness.
Month 4: Optimisation Phase
Month four often represents an optimisation phase where patients focus on fine-tuning their treatment approach and maximising their health outcomes. This period typically involves dosage adjustments, lifestyle refinements, and strategic planning for continued success.
During month four, many patients work with their healthcare provider to optimise their dosage based on their response to treatment, side effect profile, and health goals. This may involve dose increases, adjustments to injection timing, or modifications to their treatment schedule.
Lifestyle modifications become more sophisticated during month four as patients develop advanced strategies for managing their diet, exercise, and stress management. This includes more nuanced approaches to meal planning, exercise programming, and psychological support for long-term success.
Plateau management strategies become important during month four as some patients may experience temporary stalls in weight loss or other health improvements. Learning to recognise and manage these plateaus effectively is crucial for maintaining motivation and continued progress. For detailed plateau management strategies, see our Plateau Management Guide. When weight loss stalls, our Weight Loss Timeline Guide helps you understand typical progress patterns.
Social support systems become more established during month four as patients develop stronger relationships with healthcare providers, support groups, and family members who understand and support their treatment journey.
Month 5: Consolidation
Month five typically represents a consolidation phase where patients focus on maintaining their progress and preparing for long-term success. This period often involves stabilising weight loss, optimising metabolic health, and developing sustainable habits for continued treatment.
During month five, most patients experience stable, consistent progress with fewer fluctuations in appetite, energy levels, or treatment effectiveness. This stability allows for more focused attention on long-term health goals and lifestyle sustainability.
Metabolic health improvements continue during month five, with many patients reporting sustained improvements in blood sugar control, cholesterol levels, and overall metabolic function. These improvements often accompany continued weight loss and contribute to overall health and well-being.
Lifestyle integration becomes more seamless during month five as patients develop routines and strategies that feel natural and sustainable. This includes meal planning, exercise routines, and stress management techniques that support long-term health and treatment success.
Psychological adaptation continues during month five as patients become more comfortable with their new lifestyle and develop greater confidence in their ability to maintain their health goals long-term. This psychological adaptation is crucial for sustained success.
Month 6: Long-term Preparation
Month six often represents a preparation phase for long-term treatment success as patients prepare for continued treatment and develop strategies for maintaining their progress over extended periods. This period focuses on sustainability and long-term health improvement.
During month six, patients typically work with their healthcare provider to develop long-term treatment plans that address continued weight management, metabolic health improvement, and overall health optimisation. This planning is crucial for sustained success.
Lifestyle sustainability becomes a primary focus during month six as patients develop habits and routines that can be maintained over extended periods. This includes dietary strategies, exercise routines, and stress management techniques that support long-term health and well-being. For comprehensive long-term guidance, see our Long-term Use Guide.
Social and professional integration becomes more established during month six as patients develop strategies for managing their treatment in various social and professional contexts. This includes communication strategies, accommodation planning, and support system development.
Monitoring and assessment become more sophisticated during month six as patients develop advanced strategies for tracking their progress, identifying areas for improvement, and making adjustments to their treatment approach based on their individual response and health goals.
Common Experiences During Months 2-6
Understanding common experiences during months 2-6 helps you prepare for what to expect and recognise when to seek medical advice. While individual responses vary, certain patterns are commonly reported by patients during this extended treatment period.
Most patients experience consistent appetite suppression during months 2-6, though the intensity may vary slightly between individuals and over time. This effect typically becomes more stable and predictable, making meal planning and dietary adherence easier to maintain.
Weight loss patterns vary significantly during months 2-6, with some patients experiencing steady, consistent weight loss while others may experience periods of more rapid loss followed by stabilisation. Both patterns are normal and depend on individual factors including starting weight, metabolic rate, and lifestyle choices.
Energy level improvements are commonly reported during months 2-6, with many patients experiencing sustained improvements in energy, mood, and overall well-being. These improvements often accompany metabolic health improvements and contribute to overall quality of life.
Social and lifestyle adaptation continues during months 2-6 as patients become more comfortable with their treatment routine and develop strategies for managing their health goals in various social and professional contexts.
Managing Challenges and Setbacks
Effective management of challenges and setbacks during months 2-6 is crucial for maintaining treatment success and motivation. Most challenges are manageable with proper preparation, support, and strategic planning.
Weight loss plateaus are common during months 2-6 and can be managed effectively with lifestyle modifications, treatment adjustments, and psychological strategies. Understanding that plateaus are normal and temporary helps maintain motivation and commitment to treatment. For comprehensive plateau management strategies, see our Plateau Management Guide.
Social challenges may arise during months 2-6 as patients navigate social situations, family dynamics, and professional responsibilities while maintaining their health goals. Developing communication strategies and support systems helps manage these challenges effectively.
Lifestyle fatigue can occur during months 2-6 as patients work to maintain dietary restrictions, exercise routines, and other lifestyle modifications. Developing sustainable strategies and seeking support helps prevent burnout and maintain long-term success.
Treatment adherence challenges may arise during months 2-6 as patients become more comfortable with their routine and may become less vigilant about following treatment recommendations. Maintaining awareness and seeking support helps ensure continued adherence and optimal outcomes.
Optimising Your Treatment Approach
Optimising your treatment approach during months 2-6 involves working closely with your healthcare provider to maximise your health outcomes and develop strategies for long-term success. This optimisation is based on your individual response to treatment and health goals.
Dosage optimisation may be necessary during months 2-6 as your body adapts to treatment and your health goals evolve. Working with your healthcare provider to adjust your dosage based on your response, side effects, and health objectives ensures optimal treatment effectiveness.
Lifestyle optimisation involves refining your dietary strategies, exercise routines, and stress management techniques based on your experience and health goals. This optimisation helps maximise your treatment outcomes and supports long-term health improvement.
Monitoring optimisation includes developing more sophisticated strategies for tracking your progress, identifying areas for improvement, and making adjustments to your treatment approach. This optimisation helps ensure continued progress and long-term success.
Support system optimisation involves developing stronger relationships with healthcare providers, support groups, and family members who understand and support your treatment journey. This optimisation provides crucial support for long-term success.
Preparing for Long-term Success
Preparing for long-term success during months 2-6 involves developing strategies and habits that support continued treatment effectiveness and health improvement over extended periods. This preparation is crucial for sustained success and optimal outcomes.
Long-term treatment planning involves working with your healthcare provider to develop strategies for continued weight management, metabolic health improvement, and overall health optimisation. This planning addresses your individual needs and health goals.
Sustainable lifestyle development focuses on creating habits and routines that can be maintained over extended periods. This includes dietary strategies, exercise routines, and stress management techniques that support long-term health and well-being.
Support system development involves building relationships with healthcare providers, support groups, and family members who understand and support your treatment journey. This support system provides crucial assistance for long-term success.
Monitoring and assessment strategies become more sophisticated as you prepare for long-term success. This includes developing advanced approaches to tracking your progress, identifying areas for improvement, and making adjustments to your treatment approach based on your individual response and health goals.
Order Retatrutide Online
Available in 10mg vials. Select your pack size and checkout securely below.
-
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
Frequently Asked Questions
- What should I expect during months 2-6? During months 2-6, you can expect more consistent appetite suppression, stable energy levels, continued weight loss, and improved metabolic function. Side effects typically continue to diminish, and the medication’s beneficial effects become more pronounced and reliable.
- How often should I see my healthcare provider during months 2-6? Regular follow-up appointments are important during months 2-6 to monitor your progress, assess your response to treatment, and make any necessary adjustments to your treatment plan. Most patients benefit from monthly or bi-monthly appointments during this period.
- What should I do if I experience a weight loss plateau? Weight loss plateaus are normal during months 2-6 and can be managed with lifestyle modifications, treatment adjustments, and psychological strategies. Work with your healthcare provider to develop strategies for breaking through plateaus and maintaining motivation.
- How should I adjust my lifestyle during months 2-6? Focus on developing sustainable habits and routines that support your long-term health goals. This includes refined meal planning, optimised exercise routines, and improved stress management strategies that can be maintained over extended periods.
- Can I increase my dosage during months 2-6? Dosage adjustments may be appropriate during months 2-6 based on your response to treatment, side effects, and health goals. Work with your healthcare provider to determine if dosage adjustments are appropriate for your individual situation.
- What should I track during months 2-6? Continue tracking your symptoms, side effects, appetite changes, energy levels, and overall well-being. Also monitor your weight, metabolic health markers, and treatment adherence to ensure optimal outcomes and identify areas for improvement. For comprehensive tracking guidance, visit our Retatrutide Guides Hub for detailed monitoring strategies.
- How do I prepare for long-term treatment? Focus on developing sustainable lifestyle habits, building strong support systems, and working with your healthcare provider to create long-term treatment plans that address your individual needs and health goals.
- What should I do if I experience challenges or setbacks? Seek support from your healthcare provider, support groups, or family members. Most challenges are manageable with proper preparation, support, and strategic planning. Don’t hesitate to reach out for help when needed.