Mechanisms of Action Comparison
Retatrutide and Lixisenatide represent fundamentally different approaches to metabolic disease treatment, each targeting distinct hormonal pathways to achieve therapeutic effects. Understanding their mechanisms of action provides crucial insights into their comparative efficacy and potential applications in clinical practice.
Retatrutide operates as a triple hormone receptor agonist, simultaneously activating three key receptors: glucagon-like peptide-1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and glucagon. This comprehensive approach creates synergistic effects that address multiple aspects of metabolic regulation. The GLP-1 receptor activation enhances insulin secretion, suppresses glucagon release, and slows gastric emptying, while GIP receptor stimulation further amplifies insulin response and promotes glucose uptake in peripheral tissues. The glucagon receptor activation increases energy expenditure through enhanced lipolysis and thermogenesis, creating a powerful combination that maximises weight loss potential.
Lixisenatide contains a GLP-1 receptor agonist that represents a short-acting formulation designed for postprandial glucose control. As a single-receptor agonist, Lixisenatide focuses specifically on GLP-1 receptor activation, which provides established benefits including enhanced insulin secretion, reduced glucagon release, slowed gastric emptying, and appetite suppression. The short-acting nature of Lixisenatide makes it particularly effective for controlling postprandial glucose excursions, though its duration of action may limit its overall metabolic benefits compared to longer-acting GLP-1 receptor agonists.
Ready to Order?
Choose your preferred amount below, fast shipping and secure checkout.
-
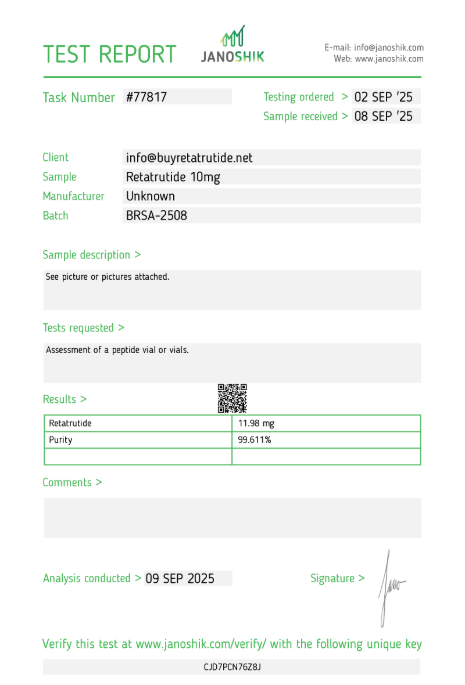
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
The fundamental difference between these mechanisms lies in their scope of action and duration of effect. Retatrutide’s triple agonist approach provides the most comprehensive coverage of metabolic pathways, potentially offering superior efficacy through synergistic receptor interactions. The addition of GIP and glucagon receptor activation creates a unique metabolic profile that enhances both weight loss and energy expenditure beyond what single-receptor agonists can achieve. Lixisenatide’s focused GLP-1 receptor activation offers a well-established mechanism with proven efficacy for postprandial glucose control, though its short-acting nature may limit sustained metabolic benefits.
Preclinical studies have demonstrated that Retatrutide’s multi-receptor activation creates additive effects that exceed the sum of individual receptor stimulation. The simultaneous activation of GLP-1, GIP, and glucagon receptors appears to create synergistic interactions that enhance both weight loss and metabolic improvements. Lixisenatide’s single-receptor activation has been extensively studied and optimised, with the short-acting formulation providing targeted benefits for postprandial glucose control while maintaining the established benefits of GLP-1 receptor stimulation.
The pharmacokinetic profiles of these agents also differ significantly. Retatrutide’s triple receptor activation requires careful dosing optimisation to balance efficacy with tolerability, as simultaneous activation of multiple pathways may increase the risk of adverse effects. Lixisenatide’s single-receptor approach has been extensively studied and optimised, with established dosing regimens that provide effective postprandial glucose control while maintaining acceptable safety profiles. The short-acting nature of Lixisenatide offers targeted benefits for meal-related glucose excursions but may require more frequent dosing compared to longer-acting alternatives.
Clinical Efficacy and Results
Clinical trial data for both Retatrutide and Lixisenatide demonstrate significant therapeutic efficacy, though through different mechanisms and with varying degrees of weight loss and glycaemic control. Phase II trials have provided compelling evidence for Retatrutide, while Lixisenatide has established efficacy through extensive clinical development and regulatory approval.
Retatrutide has shown remarkable efficacy in clinical trials, with Phase II data demonstrating up to 24% body weight reduction over 48 weeks in adults with obesity without diabetes. This represents one of the highest weight loss percentages reported for any single-agent therapy in clinical trials. The weight loss was achieved gradually and sustained throughout the study period, with participants maintaining significant reductions even at the 48-week endpoint. Beyond weight loss, Retatrutide demonstrated substantial improvements in metabolic parameters, including reductions in fasting glucose levels, improvements in insulin sensitivity, and favourable changes in lipid profiles. These comprehensive metabolic benefits position Retatrutide as a potential game-changer in obesity treatment.
Lixisenatide has demonstrated impressive efficacy in multiple clinical trials, primarily focused on postprandial glucose control in patients with Type 2 diabetes. Clinical studies have shown that Lixisenatide 20 µg significantly lowers HbA1c levels and reduces postprandial glucose excursions by approximately 5 mmol/L compared to placebo after a standard meal. While Lixisenatide also contributes to weight loss, the extent is generally more modest compared to longer-acting GLP-1 receptor agonists. The short-acting formulation provides targeted benefits for meal-related glucose excursions, making it particularly effective for patients who experience significant postprandial hyperglycaemia.
Comparative efficacy data reveals interesting patterns in patient response. Retatrutide’s triple receptor activation appears to provide more comprehensive metabolic benefits, with improvements extending beyond weight loss to include significant enhancements in insulin sensitivity and glucose metabolism. Lixisenatide’s focused GLP-1 receptor activation results in substantial postprandial glucose control with moderate weight loss, making it particularly beneficial for patients with Type 2 diabetes who require targeted meal-related glucose management. Both agents have shown the ability to maintain their therapeutic effects over extended periods, addressing critical challenges in metabolic disease management.
Patient population differences may influence the relative efficacy of these agents. Retatrutide appears particularly effective in patients with significant insulin resistance and metabolic dysfunction, where its comprehensive receptor activation provides maximal benefit. Lixisenatide may be more suitable for patients with established Type 2 diabetes who experience significant postprandial hyperglycaemia and require targeted meal-related glucose control. The clinical trial data suggests that both agents can achieve substantial therapeutic benefits, but optimal patient selection may maximise their therapeutic potential.
Long-term efficacy considerations favour both agents, though from different perspectives. Retatrutide’s comprehensive metabolic effects may provide sustained benefits beyond weight loss, potentially addressing multiple aspects of metabolic syndrome. Lixisenatide’s established track record in clinical practice provides confidence in its long-term efficacy and safety profile, particularly for postprandial glucose control. Both agents represent significant advances in metabolic disease treatment, with their distinct mechanisms offering different advantages for various patient populations.
Safety Profiles and Side Effects
Safety considerations play a crucial role in evaluating the clinical utility of both Retatrutide and Lixisenatide. Understanding their adverse event profiles helps healthcare providers make informed decisions about patient selection and monitoring requirements. Both agents have demonstrated generally favourable safety profiles in clinical trials, though their side effect patterns differ based on their distinct mechanisms of action.
Retatrutide’s safety profile reflects its triple receptor activation approach, with gastrointestinal symptoms being the most commonly reported adverse events. Nausea, diarrhoea, vomiting, and constipation occur frequently, particularly during the initial treatment period. These symptoms are typically mild to moderate in severity and tend to diminish over time as patients adjust to the medication. The gastrointestinal side effects are consistent with GLP-1 receptor activation and are generally manageable with appropriate dosing strategies and patient education. More serious adverse events are rare but can include pancreatitis, gallbladder disease, and hypoglycaemia, particularly in patients with diabetes.
Lixisenatide has demonstrated a favourable safety profile with generally mild to moderate adverse events. Similar to other GLP-1 receptor agonists, Lixisenatide may cause side effects such as nausea, vomiting, diarrhoea, and abdominal pain. These side effects are usually mild and diminish over time as patients adjust to the medication. However, there is a risk of more serious side effects, including pancreatitis and kidney problems, which require careful monitoring. The short-acting nature of Lixisenatide may result in different tolerability characteristics compared to longer-acting GLP-1 receptor agonists.
Comparative safety data reveals important differences between these agents. Retatrutide’s comprehensive receptor activation may result in more frequent gastrointestinal side effects, particularly during the initial treatment period. However, these effects are generally predictable and manageable with appropriate patient counselling and dose titration. Lixisenatide’s single-receptor approach appears to offer good tolerability, with side effect profiles similar to established GLP-1 receptor agonists. The established safety database for Lixisenatide provides confidence in its clinical use.
Long-term safety considerations remain important for both agents. Retatrutide’s triple receptor activation requires ongoing monitoring for potential effects on multiple organ systems, including the pancreas, gallbladder, and cardiovascular system. Lixisenatide’s single-receptor mechanism has been extensively studied in clinical trials and real-world use, providing a comprehensive understanding of its long-term safety profile. Both agents require careful patient selection and monitoring, particularly in patients with pre-existing medical conditions that may be affected by their mechanisms of action.
Patient-specific factors significantly influence the safety profiles of these agents. Retatrutide may be more suitable for patients who can tolerate initial gastrointestinal side effects in exchange for potentially greater weight loss efficacy. Lixisenatide may be preferable for patients who require effective treatment with established safety profiles, particularly those with Type 2 diabetes who need targeted postprandial glucose control. The safety profiles of both agents support their potential as valuable additions to the metabolic disease treatment armamentarium, with appropriate patient selection and monitoring being key to optimising their therapeutic benefits while minimising risks.
Regulatory Status and Availability
The regulatory landscape for Retatrutide and Lixisenatide reflects their different stages of development and approval. Understanding their current regulatory positions provides insight into their availability, pricing, and potential timeline for expanded clinical use.
Retatrutide is currently undergoing Phase III clinical trials, representing the final stage of clinical development before potential regulatory approval. The compound has progressed through Phase I and Phase II trials with promising results, demonstrating both efficacy and safety in multiple patient populations. The Phase III programme is designed to confirm the efficacy and safety findings from earlier trials in larger, more diverse patient populations. Regulatory submissions are anticipated following successful completion of the Phase III trials, with potential approval timelines dependent on the specific regulatory pathways pursued in different jurisdictions.
Lixisenatide has achieved regulatory approval in Europe since 2013 for the treatment of Type 2 diabetes, representing a significant milestone in its clinical development. The approval was based on comprehensive clinical trial data demonstrating efficacy in postprandial glucose control and moderate weight loss. Lixisenatide is marketed under the brand name Adlyxin in some regions and represents an established GLP-1 receptor agonist with proven safety and efficacy profiles. The established regulatory approval provides confidence in Lixisenatide’s safety and efficacy profile, making it available for clinical use in approved indications.
Market availability and pricing considerations differ significantly between these agents. Retatrutide remains investigational and is not commercially available, with access limited to clinical trial participation. Lixisenatide is commercially available in approved markets, with established pricing and reimbursement structures. The commercial availability of Lixisenatide provides immediate access for patients with Type 2 diabetes, while Retatrutide’s investigational status limits current clinical applications.
Regulatory considerations for both agents include the evaluation of their risk-benefit profiles, particularly given their novel mechanisms of action. Retatrutide’s triple receptor activation approach represents a significant advancement in obesity treatment, but also introduces regulatory complexity due to its comprehensive mechanism. Lixisenatide’s single-receptor targeting has been successfully evaluated and approved, providing a regulatory pathway that may inform future multi-receptor agonist approvals.
Future regulatory developments may expand the approved indications for both agents. Retatrutide’s regulatory pathway will likely focus on obesity treatment, given its impressive weight loss efficacy in clinical trials. Lixisenatide may receive expanded approval for additional indications, building on its established safety and efficacy profile. These regulatory developments will significantly impact the clinical availability and accessibility of both agents for patients requiring metabolic disease therapy.
Head-to-Head Comparison
Direct comparison between Retatrutide and Lixisenatide reveals distinct advantages and considerations for each agent. While head-to-head clinical trials are limited, available data provides valuable insights into their relative efficacy, safety, and clinical utility. Understanding these comparative aspects helps healthcare providers make informed decisions about optimal therapy selection for individual patients.
Efficacy comparisons demonstrate that Retatrutide achieves superior weight loss as monotherapy, with up to 24% body weight reduction compared to Lixisenatide’s more modest weight loss effects. However, this comparison must be interpreted cautiously given differences in study duration, patient populations, and regulatory status. Retatrutide’s triple receptor activation provides comprehensive metabolic benefits beyond weight loss, including significant improvements in insulin sensitivity and glucose metabolism. Lixisenatide’s single-receptor approach offers substantial postprandial glucose control with moderate weight loss, making it particularly beneficial for patients with Type 2 diabetes who experience significant meal-related hyperglycaemia.
Safety comparisons reveal important differences in side effect profiles and tolerability. Retatrutide’s comprehensive receptor activation may result in more frequent gastrointestinal side effects, particularly during the initial treatment period. However, these effects are generally predictable and manageable with appropriate patient counselling and dose titration. Lixisenatide’s single-receptor approach appears to offer good tolerability, with side effect profiles similar to established GLP-1 receptor agonists. The established safety database for Lixisenatide provides confidence in its clinical use.
Regulatory status represents a significant differentiator between these agents. Lixisenatide has achieved regulatory approval in Europe since 2013 for Type 2 diabetes treatment, providing immediate clinical availability and established safety profiles. Retatrutide remains investigational, limiting current clinical applications to clinical trial participation. This regulatory difference significantly impacts patient access and healthcare provider confidence in prescribing these agents.
Patient selection considerations favour different agents for different populations. Retatrutide may be optimal for patients with significant insulin resistance and metabolic dysfunction who can tolerate initial gastrointestinal side effects for potentially greater weight loss efficacy. Lixisenatide may be preferable for patients with established Type 2 diabetes who experience significant postprandial hyperglycaemia and require targeted meal-related glucose control. The choice between these agents should be individualised based on patient characteristics and treatment goals.
Long-term considerations suggest different advantages for each agent. Retatrutide’s comprehensive metabolic effects may provide sustained benefits beyond weight loss, potentially addressing multiple aspects of metabolic syndrome. Lixisenatide’s established track record in clinical practice provides confidence in its long-term efficacy and safety profile, particularly for postprandial glucose control. The optimal choice may depend on individual patient priorities regarding efficacy versus established safety profiles and regulatory approval status.
Clinical Trial Limitations
Understanding the limitations of clinical trial data is crucial for interpreting the comparative efficacy and safety of Retatrutide and Lixisenatide. While both agents have demonstrated promising results in clinical trials, several factors limit the generalisability of these findings and highlight the need for continued research and clinical evaluation.
Study design variations significantly impact the comparability of clinical trial results between Retatrutide and Lixisenatide. Retatrutide trials have typically employed longer study durations, with some extending to 48 weeks, while Lixisenatide trials have varied in duration depending on the specific study objectives and regulatory requirements. These differences in study length make direct efficacy comparisons challenging, as weight loss patterns may differ over time. Additionally, patient population characteristics vary between studies, including differences in baseline body mass index, age, gender distribution, and presence of comorbidities such as diabetes.
Dosing regimen differences further complicate comparative analysis. Retatrutide trials have explored various dosing strategies, with optimal dosing still being determined through ongoing research. Lixisenatide trials have established effective dosing regimens, but optimal dosing for both agents remains subject to ongoing investigation. These dosing variations may influence both efficacy and safety outcomes, making it difficult to establish definitive comparative profiles.
Patient selection criteria create additional limitations in generalising trial results to broader clinical populations. Clinical trials typically employ strict inclusion and exclusion criteria that may not reflect real-world patient populations. Patients with significant comorbidities, those taking multiple medications, or those with complex medical histories may be underrepresented in clinical trials. This limits the applicability of trial results to diverse clinical settings where patients often present with multiple health conditions.
Long-term safety and efficacy data remain limited for Retatrutide, as most clinical trials have been of relatively short duration. Obesity is a chronic condition requiring long-term management, and the sustainability of weight loss and long-term safety profiles beyond the trial periods remain uncertain. Lixisenatide has more extensive long-term data through its regulatory approval process and real-world use, but comprehensive long-term data for both agents continues to be collected.
Real-world effectiveness may differ from clinical trial efficacy due to various factors including patient adherence, healthcare provider experience, and practical implementation challenges. Clinical trials provide controlled environments with close monitoring and support, which may not be replicable in routine clinical practice. The gap between clinical trial efficacy and real-world effectiveness represents an important consideration for healthcare providers and patients.
Related Research Comparisons
The landscape of metabolic disease treatment continues to evolve with multiple investigational compounds targeting different pathways. Understanding how Retatrutide and Lixisenatide compare to other emerging therapies provides valuable context for their potential clinical applications and helps identify optimal treatment strategies for different patient populations.
Other Lixisenatide formulations provide important context for evaluating Lixisenatide’s position in the treatment landscape. The Retatrutide vs Adlyxin comparison examines the branded formulation of Lixisenatide, while comparisons with other short-acting GLP-1 receptor agonists offer insights into the broader category. These comparisons demonstrate the progression from single-receptor to multi-receptor approaches, with Retatrutide representing the most comprehensive multi-receptor agonist currently in development.
Other short-acting GLP-1 receptor peptides offer additional insights into the evolving landscape of metabolic disease treatment. The Retatrutide vs Exenatide comparison explores short-acting GLP-1 agonists, while the Retatrutide vs Byetta analysis examines twice-daily exenatide formulations. The Retatrutide vs Liraglutide comparison evaluates daily GLP-1 agonists. These comparisons highlight the diverse approaches being investigated for metabolic disease treatment.
Multi-receptor agonist comparisons provide valuable context for Retatrutide’s position in the treatment landscape. The Retatrutide vs Tirzepatide comparison examines dual GLP-1/GIP receptor agonists, while comparisons with traditional therapies like Retatrutide vs Metformin explore established treatment approaches. These comparisons demonstrate the progression from single-receptor to multi-receptor approaches, with Retatrutide representing the most comprehensive triple agonist currently in development.
Combination therapy approaches represent a significant area of research interest, particularly for agents like Lixisenatide that have established safety profiles. The potential for combining different receptor agonists or adding other therapeutic modalities continues to be explored. These combination approaches may provide enhanced efficacy while maintaining acceptable safety profiles, offering new possibilities for metabolic disease treatment.
Future research directions continue to explore novel mechanisms and combination approaches. The development of additional multi-receptor agonists and the optimisation of existing compounds represent ongoing areas of investigation. These research efforts highlight the dynamic nature of metabolic disease treatment research and the potential for continued innovation in this field.
Order Retatrutide Online
Available in 10mg vials. Select your pack size and checkout securely below.
-
Reta 10mg 3 Vials
£195.00Independently verified COA. UK stock, worldwide delivery. For lab use only.
Frequently Asked Questions
General Questions
- What is the main difference between Retatrutide and Lixisenatide?
Retatrutide is a triple hormone receptor agonist that simultaneously activates GLP-1, GIP, and glucagon receptors, while Lixisenatide is a short-acting GLP-1 receptor agonist designed for postprandial glucose control. - Which agent provides better weight loss results?
Retatrutide achieves superior weight loss as monotherapy with up to 24% body weight reduction, while Lixisenatide provides more modest weight loss effects with substantial postprandial glucose control benefits. - Are both agents currently available for clinical use?
Lixisenatide is approved in Europe since 2013 for Type 2 diabetes treatment and commercially available, while Retatrutide remains investigational and is only accessible through clinical trial participation.
Mechanism Questions
- How does Retatrutide’s triple receptor activation work?
Retatrutide simultaneously activates GLP-1, GIP, and glucagon receptors, creating synergistic effects that enhance insulin secretion, suppress appetite, slow gastric emptying, and increase energy expenditure. - What makes Lixisenatide’s short-acting formulation unique?
Lixisenatide is designed for postprandial glucose control, providing targeted benefits for meal-related glucose excursions while maintaining established GLP-1 receptor benefits. - Can these agents be used together?
While both agents target GLP-1 receptors, their combination has not been extensively studied and may increase side effect risks without proportional efficacy gains.
Safety Questions
- What are the most common side effects of Retatrutide?
The most common side effects include gastrointestinal symptoms such as nausea, diarrhoea, vomiting, and constipation, which are typically mild to moderate and diminish over time. - How does Lixisenatide’s safety profile compare?
Lixisenatide has demonstrated a favourable safety profile with generally mild to moderate gastrointestinal side effects, similar to established GLP-1 receptor agonists. - Are there any serious safety concerns with either agent?
Both agents have demonstrated generally favourable safety profiles in clinical trials, though Retatrutide’s long-term safety data is still being collected through ongoing clinical trials.
Clinical Questions
- Which patients might benefit most from Retatrutide?
Retatrutide may be optimal for patients with significant insulin resistance and metabolic dysfunction who can tolerate initial gastrointestinal side effects for potentially greater weight loss efficacy. - Who might be better suited for Lixisenatide?
Lixisenatide may be preferable for patients with established Type 2 diabetes who experience significant postprandial hyperglycaemia and require targeted meal-related glucose control. - What is the expected timeline for Retatrutide availability?
Retatrutide is in Phase III trials with potential availability within the next few years, assuming successful trial completion and regulatory approval.
Conclusion
The comparison between Retatrutide and Lixisenatide highlights the evolving landscape of metabolic disease treatment, with both agents representing significant advances in therapeutic approaches. Retatrutide’s triple receptor activation offers comprehensive metabolic benefits with superior weight loss efficacy, while Lixisenatide’s single-receptor targeting provides substantial postprandial glucose control with convenient dosing and established safety profiles.
Clinical trial data demonstrates that both agents can achieve substantial therapeutic benefits, with Retatrutide achieving up to 24% body weight reduction and Lixisenatide providing significant postprandial glucose control with moderate weight loss. The choice between these agents should be individualised based on patient characteristics, regulatory status, and treatment goals. Retatrutide may be optimal for patients with significant metabolic dysfunction who can tolerate initial side effects, while Lixisenatide may be preferable for patients with Type 2 diabetes who require targeted meal-related glucose control.
As Retatrutide progresses through Phase III clinical trials and Lixisenatide continues to demonstrate real-world efficacy, continued research will provide additional insights into their long-term safety and efficacy profiles. The regulatory approval of Lixisenatide provides immediate clinical availability, while Retatrutide’s investigational status offers the potential for even greater efficacy once approved. Healthcare providers and patients should stay informed about the latest developments in this rapidly evolving field as these agents continue to advance metabolic disease treatment options.
For concentration calculations, visit our research calculator. For handling guidelines, see our information hub. Find verified suppliers for Lixisenatide and Retatrutide research materials with COA documentation.
For laboratory research use only. Not for human consumption. No medical advice. Information relevant to the United Kingdom.